Paragon Glucose Top Tips
Continuous Glucose Monitoring
Jane Scott, RCVS Advanced Practitioner in Small Animal Medicine, discusses a diabetic patient who was proving difficult to control on insulin therapy and will give some tips on diagnostic tools that can be used when approaching diabetic patients.
The clinical presentation
Macey is a 6 year old FN Labrador who presented to the medical team at Paragon Veterinary Referrals last year. She had been diagnosed with diabetes mellitus in 2017 when she had presented to her local practice with PU/PD, lethargy and weight loss. She was referred last year following a collapsing episode on a walk. She had also lost weight and had occasional nocturia. She was receiving 10iu (0.5iu/kg) of glargine insulin twice a day and the dose had been gradually increased based on spot glucose measurements.
What should I do next?
The first step in approaching a diabetic patient is to check owner compliance with the insulin< storage and administration. We were satisfied that administration technique was appropriate.
Routine bloods were performed to assess for any concurrent disease that could be affecting stabilisation. Other than mild liver enzyme elevations (consistent with diabetes mellitus) these were unremarkable. Specific pancreatic lipase was within normal limits. Fructosamine was 641 umol/l consistent with poor control. Abdominal ultrasound revealed no structural abdominal disease and urinalysis including culture was unremarkable except for glucosuria.
What further information do I
need to know?
When assessing response to insulin therapy we need to establish if the dose of insulin is appropriate (determined by the blood glucose nadir), the length of action of the insulin (determined by how long over the day the blood glucose is in our desired range) and whether the peak insulin effect coincides with the postprandial hyperglycaemia.
What tools are available to me to further assess patient response to insulin therapy?
Spot blood glucose measurements – these do not answer our questions here so are of limited value
• Fructosamine – this is a measure of the average blood glucose over a period of time. Measuring fructosamine has the advantage that only one sample is required and there is no period of hospitalisation but it is important to remember that as this is an average, a patient that is having very high and very low blood glucose readings can have a fructosamine within normal range. It also does not tell us the nadir or peak. The value can be affected by stress and also serum/plasma protein levels and concurrent disease (such as hyperthyroidism in cats)
• A serial blood glucose curve – this is a useful tool as it will answer the questions above, however, the disadvantage is that multiple venepunctures are required and usually a period of hospitalisation (with consequent stress affecting the results)
• Interstitial glucose monitoring – a relatively new tool available to us is the Freestyle Libre interstitial glucose monitoring device (Abbott, UK). The device monitors interstitial glucose continuously by means of a sensor placed in the subcutaneous tissue. An electrochemical reaction between the electrode of the sensor and glucose in the interstitial fluid produces a current which is recorded by the device. A reading is taken every 30 seconds and the data is stored and subsequently downloaded to a computer where a graph can be produced.
There is good correlation between readings and conventional blood glucose measurements and the continuous monitoring avoids peak or nadir results being missed between two conventional blood glucose samples being taken.
How do I place the device?
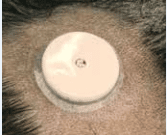
The device is easily and non-invasively placed and is tolerated well with minimal signs of irritation
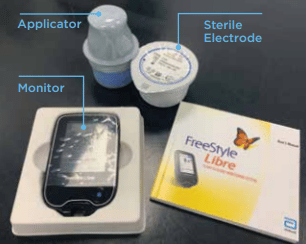
The monitor is used to scan the electrode once in situ and stores the data (an app is also available so a smartphone can also be used to record the data).
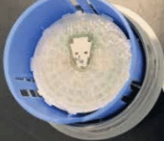
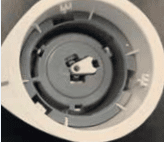
The electrode is inserted onto the end of the applicator. Hair is clipped and the skin cleaned with an alcohol wipe.
The applicator with the electrode attached is placed against the skin and the electrode fired into the subcutaneous tissue. The electrode is secured with tissue adhesive and a dressing. A stockinette dressing can be used to further protect the device.
What was the result in Macey?
Macey had an interstitial glucose monitoring device placed and was discharged to her home environment so normal routine could be continued. The device can be left in situ for up to 14 days.
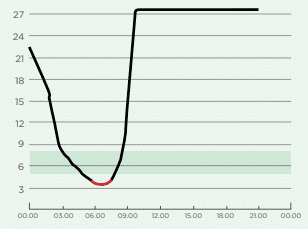
The curve generated revealed hypoglycaemia following insulin administration followed by a rebound hyperglycaemia (Somogyi effect). Macey’s insulin dose was in fact too high and following a< 20% dose reduction she stabilised.
For which patients should I consider an interstitial glucose monitor?
Where stress is thought to be affecting the results of a blood glucose curve or fructosamine
• There are concerns about owner noncompliance at home (for example good blood glucose curve results in the practice but clinical signs and fructosamine suggest poor control)
• Patients with continued clinical signs despite increasing doses of insulin
• Patients hospitalised with DKA that are requiring regular monitoring of their glucose It is always important to remember to interpret the results from the device in combination with clinical signs and examination findings.
The medical team at Paragon Veterinary Referrals are always very happy to discuss any diabetic cases who are not responding well to treatment and may benefit from implantation of an interstitial device.
