Patella Luxation Physiotherapy For Clients
Patella luxation (kneecap dislocation)
What is it?
You may have noticed your dog skipping or ‘bunny hopping’ when trotting or running. There are several conditions that this may be associated with but one of the most common is patella luxation. The patella will most commonly come out of its groove and move to the inside of the stifle (knee) joint. In some patients the patella moves to the outside instead. As time goes by this may occur more frequently.
Over time the action of the patella luxating causes wear and tear of the cartilage in the joint. This will result in poor function and pain. At this point lameness will develop which can continue to worsen.
How does it happen?
To understand what is happening we need to have a look at the anatomy of the hindlimb
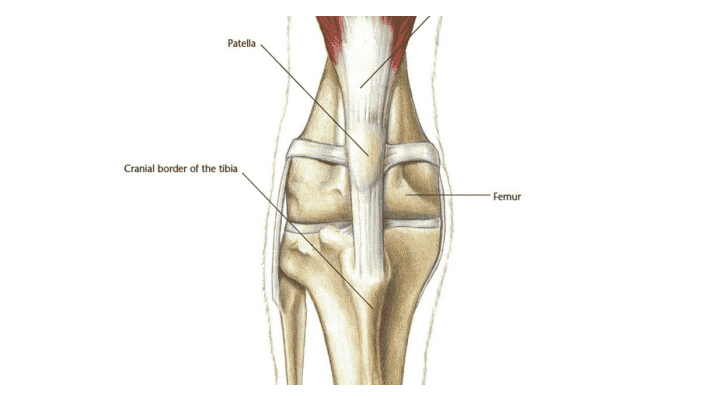
The patella is attached to the bottom of the quadriceps muscles which are the large thigh muscles. It is connected to the front of the tibia at a point called the tibial tuberosity. Normally it sits in a groove at the bottom of the femur where it helps
with extending the knee joint.
During patella luxation the patella slips out of the groove. This is what leads to the skipping or bunny hopping that is usually associated with the simpler forms of luxation. With increasing severity comes greater degrees of lameness and loss of function. For the patella to luxate it has to be pulled out of its normal position by the muscle that it is attached to. Muscles and tendons can only pull in a straight line and the patella will go wherever they pull it. If there are bony deformities in the femur or the tibia then the patella will start to dislocate. The deformities can be either a bend and/ or twist in the femur or tibia. The more severe deformities will result in more complex patella luxation that may need more advanced techniques to resolve it.
How is it diagnosed?
The symptoms of skipping and bunny hopping are good indicators. When examining your pet, we can feel the knee joint and will be able to push the patella out of its usual position in certain positions. In the more severe forms of patella luxation the patella may be permanently out of the groove and can be felt on the inside of the leg.
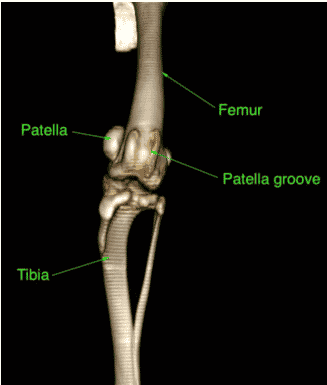
The next step is usually radiographs (x-rays) or a CT scan. The choice is dependent on the severity of the problem. These images will allow assessment of the bony deformities, the position of the patella and the depth of the groove that the patella sits in.
How is it treated?
Most cases of patella luxation require surgery. Certainly, those that are showing signs of skipping, bunny hopping or lameness should be considered for surgery as the condition is likely to progress over time. The condition may also increase the risk of developing cruciate ligament disease. Patella luxation surgery usually involves several parts:
• In many patients the groove that the patella sits in is too shallow. In these cases, we remove deepen the groove (this is called a sulcoplasty). This will allow the patella to sit in a better position.
•Tibial tuberosity transposition. This part of the procedure involves cutting the front of the tibia (tuberosity) and moving it over into a better position that helps with the alignment of the patella and muscles. The cut section of bone is then secured with pins and wire.
• Soft tissue procedures. The tissues on inside of the knee (if the luxation is towards the inside) may be cut to release fibrous (scar) tissue. On the outside of the knee the tissues may be tightened to help with the alignment of the patella.
• In more advanced cases such as in the CT image above then more invasive techniques may be required. This may involve cutting the femur and or tibia in a procedure known as a corrective osteotomy. Usually the cut bone will be secured with a bone plate and screws.
• Patella groove replacement. In some patients the groove is very arthritic or the patella has a painful ulcer. These patients may benefit from an artificial replacement that reduces pain and maintains good function.
What outcome can be expected?
Most patients can be expected to do very well following corrective surgery. After a period of rest and controlled exercise they should be able to return to normal exercise. Recovery usually takes approximately 2 months.
In the long term there should be less progression of arthritis than would have occurred without surgery. There should also be a reduced risk of developing cruciate ligament disease.
